What affects how likely you are to die from the novel coronavirus?
The answer is clear: The older you are and the more health problems that afflict you, the more likely you won’t make it.
We can’t do anything about getting older except age with grace and tolerate the excesses of youth (as long as they honor social distancing). Health problems, however, are another thing, because they may have causes that can be prevented and/or treated.
Which health problems stand out as likely to make your COVID-19 experience deadly?
Diabetes, obesity, heart disease, high blood pressure, and reduced immunity, among others. These are diseases that develop over a lifetime, and so you won’t be able to change them in the course of the current pandemic. If you have one or more of these diseases, protect yourself by taking your meds as directed, and follow all the social distancing recommendations issued by public health officials.
But if there’s one certainty about this, it is that this will not be the last pandemic. That’s guaranteed by a growing human population, global integration of society (especially by airplanes), and features of today’s civilization that make it more likely that animal diseases will infect humans. Among these are habitat destruction which brings wild animals closer to humans, wild animal food markets like those in Wuhan, and industrial confinement of livestock in close quarters as occurs throughout the U.S. as well as elsewhere in the world.
What can we do in anticipation of the next pandemic to lower the mortality rate once it gets underway? We need to reduce the frequency and severity of the health problems that make us more likely to die.
These are complex, multifactorial diseases that have been surging in their own epidemics over the last half-century. More people suffer from them, and they strike younger and younger people. They are proving to be tough nuts to crack for traditional public health approaches.
That said, over the past two decades we have seen a tremendous increase in the types of disease that makes us more vulnerable to pathogens.
A global public health threat
A huge body of research into a family of chemicals that alter hormone action, called endocrine-disrupting chemicals, has increasingly established them as significant contributors to the risk of these very diseases: diabetes, obesity, heart disease, high blood pressure, reduced immunity, and more.
There is always uncertainty in science, but the evidence has become strong enough that the Endocrine Society, the world’s largest professional association of medical and research endocrinologists, considers reducing endocrine-disrupting chemicals’ impacts to be one of their highest public health goals. Endocrinologists are the go-to health professionals for these diseases, both for figuring how to treat them and understanding how they cause effects.
In 2012, the World Health Organization and the United Nations Environment Program released a report concluding that endocrine-disrupting chemicals are a global public health threat.
The science has only grown stronger since then.
Thousands of scientific papers have been published in the last 20 years linking endocrine-disrupting chemical exposure to the very comorbidities that increase the risk of dying from COVID-19.
Some of the chemicals highlighted in this research are bisphenols like BPA, phthalates (plasticizers), perfluorinated (forever) chemicals, flame retardants, PCBs and a variety of new and old pesticides.
One of the most disturbing studies found that vaccines don’t work as well in children who had high levels of perfluorinated chemicals, PFOS and PFOA, in them as infants
In 2020 each of us carries a collection of these chemicals in our bodies, including in our blood, tissues and organs.
There is much more in us now than there was even 30 years ago. No one is uncontaminated, including unborn babies.
Given what the research tells us, it’s not surprising that with higher levels of endocrine-disrupting chemical exposure, the endocrine-related adverse health effects noted above have surged as public health threats.
Nor is it surprising that the effects are being seen in younger and younger adults, and now even in teenagers.
Hitting the “trifecta” of health, money, and fewer deaths
What will that take to weather the next pandemic, and the next?
First, regulatory agencies like the U.S. Food and Drug Administration and the Environmental Protection Agency need to use modern science to establish what is safe and what is not. Their approaches today do not reflect modern endocrinological science. They are mired in science from a previous century.
Second, we need the next generation of materials used in consumer products to be inherently safer than what we have today, because many of those products contain, and emit, endocrine-disrupting chemicals.
The good news is that endocrine-disrupting chemical science has advanced so substantially over these past two decades that chemists can use it to design safer materials.
And they can make money in the process, because, increasingly, consumers want to be confident that what they are bringing into their homes and their bodies is safe.
This is a clear path forward. Chemical inventors and chemical companies make money. People are healthier. Fewer people die in the next pandemic. Sounds like we can hit the trifecta.
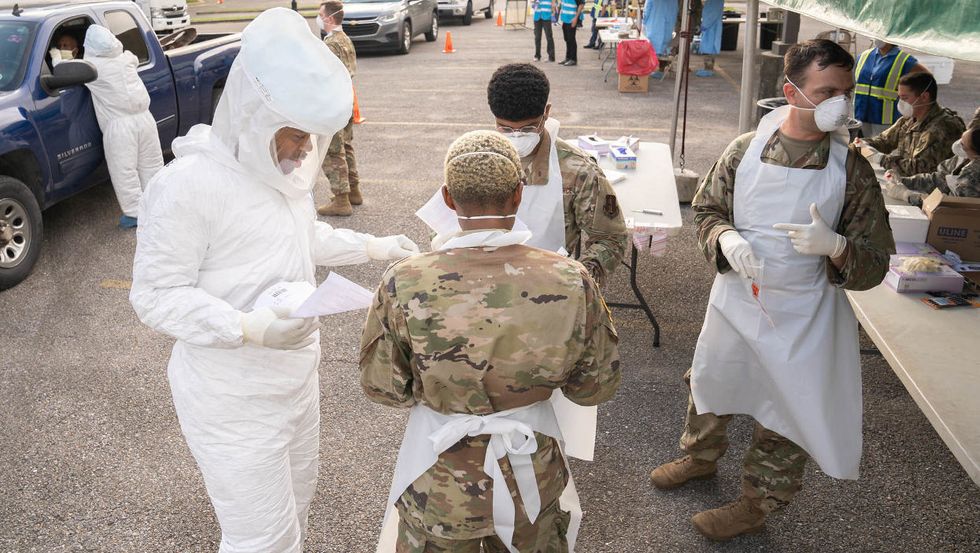
Banner Photo: Louisiana National Guard Soldiers and Airmen test first responders for COVID-19 infections at Louis Armstrong Park, New Orleans, Louisiana, March 20, 2020. (Credit: The National Guard)
Pete Myers is the founder and chief scientist of Environmental Health Sciences, publisher of EHN.org and DailyClimate.org